By Manuel Guzmán
Manuel Guzmán is Professor of Biochemistry and Molecular Biology at Complutense University of Madrid, member of the Spanish Royal Academy of Pharmacy, and member of the Board of Directors of the International Association for Cannabinoid Medicines. His research focuses on the study of the mechanism of action and therapeutic properties of cannabinoids, especially in the nervous system. This work has given rise to more than one hundred publications in specialized international journals, as well as to several international patents on the possible therapeutic applications of cannabinoids as anticancer and neuroprotective drugs. He routinely collaborates with scientific reviewing and funding agencies.
Many clinical studies that have supported the therapeutic use of a specific drug in a specific disease have been carried out because preclinical evidence about it existed previously (i.e. evidence based on established disease models in experimental animals such as mice or rats). In fact, today it would be unthinkable to undertake the very expensive clinical trials associated with any disease, especially if it is chronic and complex, in the absence of such preclinical studies. However, the (bitter) experience of recent decades reveals that, in the case of certain diseases of very high incidence and/or morbo-mortality, the numerous studies carried out with animal models have been practically unsuccessful in terms of clinical translation.
A dramatic example of this dichotomy between basic research and clinical reality is that of neurodegenerative diseases, primarily with Alzheimer's disease. A recent review of the subject reviews some 300 different treatments that have enabled this disease to be cured or improved in transgenic mice models. To date however, Alzheimer's disease has few palliative treatments (the few that exist are also ineffective) and, as is well known, there is no treatment that is not curative but that modifies (at least minimally) the course of the disease.In this bleak panorama, very powerful pharmaceutical companies have announced that they will stop altogether (for example, Pfizer) or significantly (for example, Roche, Lilly and Merck) their Alzheimer's disease therapy programmes to, presumably, focus on ailments for which their investments are more productive.
Why is there such a drastic difference between mice and humans? Well, essentially because the "real" Alzheimer's disease; that is, in humans, is much more complex and multifactorial (with numerous alterations, including genetic and acquired, neuronal, vascular, metabolic, endocrine, immune, etc.) that Alzheimer's disease models in mice (based exclusively on one or very few genetic mutations and without genetic or environmental variability between individuals). The course of Alzheimer's disease in humans, even in its clinically asymptomatic phase, is much slower (years-decades) than in Alzheimer's disease models in mice (weeks-months). Thus, when symptoms appear and it is diagnosed, the damage that the disease has already produced in human nervous tissue is irreversible and no medication can counteract it. In mice, by contrast, researchers can predict the course of (the model of) the disease and intervene at the desired time, even in asymptomatic stages. What's more, mouse biology is significantly more robust than human biology. They can, for example, regenerate tissue (including nervous tissue), trigger immune responses (which would act as "vaccines") and detoxify drugs (and, for both, tolerate them at high doses) much more effectively than humans do.
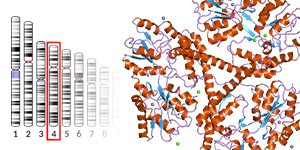
All this, as is logical, is a reminder that extraordinary caution must be taken in extrapolating the findings of basic research to clinical practice. For example, headlines that the media customarily expound, such as "Scientists discover that the drug X cures Alzheimer's disease" (or amyotrophic lateral sclerosis, or diabetes, or cancer), should be qualified to "Scientists discover that drug X attenuates the symptoms of Alzheimer's disease in the mice model." As is already well known, these "X drugs" are sometimes cannabinoids. And numerous preclinical studies on Alzheimer's disease and other neurodegenerative diseases have shown the palliative action as well as the neuroprotective power of cannabinoids in mouse models, which has aroused great expectations about their possible clinical usefulness. However, the controlled clinical studies carried out so far have not shown noticeable beneficial effects of cannabinoids (despite being safe overall and well tolerated) in the different motor, cognitive, behavioural and neuropsychiatric scales analysed, with some symptomatic relief exceptions such as seizures in refractory paediatric epilepsies, spasticity and neuropathic pain in multiple sclerosis, and various parameters of general quality of life in these or other neurodegenerative diseases (all of which, on the other hand, is highly positive in the current devastating panorama of these diseases).
In addition to the aforementioned biological, pathological and experimental factors, this discrepancy between basic and clinical research may also be due to inadequate design of the clinical trials carried out so far, which have been aimed at assessing the safety of cannabinoids rather than their efficacy. In this sense, it seems logical to suggest that future clinical trials with cannabinoids are carried out at earlier stages of the disease under study and for longer periods of treatment. It could also be useful to know the pattern of cannabis use by patients with neurodegenerative diseases and to have a biomarker related to cannabinoid receptor activity during the progression of these diseases. In summary, the safety and tolerability shown by different cannabinoids in the clinical studies carried out so far should encourage more exhaustive future trials to evaluate whether these compounds could be used as therapeutic agents for treating aggressive neurodegenerative and oncological diseases, both of which are the focus of intense research in the field of cannabinoids.