By Mariano Garcia de Palau

Born in Barcelona, 17 February 1956. Graduated in medicine and surgery from the University of Barcelona in 1979. For 38 years has worked as an emergency physician in the area of occupational medicine. He became interested in cannabis by chance, and for the last 15 years has studied its therapeutic uses.
Currently he continues to advise on cannabinoid treatments and performs clinical work with patients, collaborates with various organizations and associations, serves as Senior Consultant for Grupo Curativa Colombia and is a spokesperson for the Spanish Medical Cannabis Observatory.
Probably, cancer is the most common cause of death in industrialised countries. All the cells of our body multiply according to the information contained in their genetic code. Following these instructions that are encoded in the genes, they can be divided giving rise to healthy and functional cells in each of the different tissues of our body.
What happens when genetic information is altered for any reason?
That the resulting cell is abnormal and it does not look like the normal cells in that tissue, as well as growing much faster and also all the cells that come from it. There has been a mutation in that cell or cells. An alteration in the genome. A change in the genetic information, which will give rise to abnormal cells that will multiply according to that incorrect information. It should be noted that usually a single mutation does not lead to a cancer cell, it must produce more than one mutation to produce the neoplastic cell that generates an incorrect cell line.
A tumour has been formed that, after being studied by means of different techniques, CT, MRI, biopsy and cytology analysis will be classified as benign or malignant.
Malignant tumours, tend to be fast-growing, the faster the worse the prognosis in general. There is also another criterion for classification purposes, the specificity of their cells. The more primitive the cancerous cells are, that is, the less they resemble normal cells in the tissue they come from, the worse the prognosis with regard to malignancy. Cancers that occur in young people can be more aggressive in general than those that appear in older people.
How can a change in the genetic information of a cell be caused?
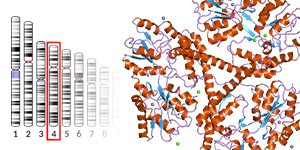
It can be caused by different factors, we can induce mutations for example by physical agents, such as exposure to ionising radiations or radioactive isotopes, chemical agents, such as those arising from the combustion of a cigarette, or viruses that cause on infecting cells of our body, an alteration in the chromosomal DNA, which gives rise to tumour cells. There are probably many more factors related to the cancer disease, such as quality in food products, or exposure to new compounds generated by industry. Even solar radiation is generating more and more skin cancers. Cells derived from the cancer stem cell multiply with incorrect information, the result of genetic mutations.
Under normal conditions, a cell that suffers irreparable damage self induces suicide, which is called apoptosis or induced cell death. This mechanism ensures that the cells that are no longer useful for our organism die in an induced manner, and are not replicated incorrectly, forming a new tissue, a tumour.
It should also be noted that, although treatments with chemotherapy agents, or radiation therapy, are without doubt very toxic and aggressive for the patient, given the advances in tumour markers, treatments are increasingly more specific and selective as regards cellular targets, which, ultimately, consists of selectively eliminating cancer cells without affecting other healthy cells in our body. But obviously the treatment of cancer in its various forms remains a challenge today.
Can cannabinoids be effective against any type of cancer?
We know that there are cannabinoids with antineoplastic or antiproliferative properties. We are even also aware of some of the mechanisms of action at the molecular level, which makes it easier to be able to predict how they act and their therapeutic effects, in relation to the possible side effects which, as we know, most medicines have, including of course chemotherapy agents, which in this case are one of the most toxic treatments to be subjected to for treating the cancer disease.
Cannabinoids inhibit the formation of new vessels in the tumour, which determines that, on not receiving sufficient blood to grow, their growth is inhibited. This phenomenon is called the inhibition of angiogenesis.
Cannabinoids, also, induce apoptosis or cell suicide of tumour cells, while respecting the viability or survival of healthy cells. There are different studies that prove it. This specificity of action, only at the level of cancer cells, is the one that is sought with chemotherapy agents, which only target cancer cells, respecting the healthy ones. Properties are also described in terms of reduction of possibilities of metastases when using cannabinoids. It is clear, therefore, that they have antineoplasic properties. It has been found that CBD specifically inhibits the action of a protein called ID, the presence of which determines greater aggressiveness and possibilities of tumour metastasis. This protein appears in several subtypes, of which ID1 and ID3 are inhibited by the CBD. They are precisely the subtypes that we have to inhibit in cancer processes.
However, we must reflect on a very important issue, most studies on the use of cannabinoids in different types of cancer come from preclinical research, with experimental animals, basically selected mice, and of course, even though we share 93% of genes, their immune system is not at all similar to ours with regards to efficiency and complexity.
We can access clinical trials, but they tend to be scarce and with not enough patients to provide extrapolated and conclusive results. This situation has been spurred by the legal situation of the use of cannabis in the different countries, it is very difficult to investigate with illegal substances.
Cancer is not a single clinical entity, there are more than 100 different cancers and each one is different from the rest in many respects. Although the patient has in general similar symptoms in many cases, pain, anxiety, insomnia, weight loss, each type of cancer affects different types of cells, tissues and organs, and therefore the symptoms will be different depending on the type of cancer.
For example, a brain cancer probably generates epilepsy, headache, neurological disorders as specific symptomatology.
Given the characteristics of the pharmaceutical industry, and the methodology of clinical trials, which are very costly in time and money, we currently do not have information that is actually proven and tested with the methodology requested by the scientific community.
We do not know exactly what combination of cannabinoids is the most appropriate for each type of cancer, nor do we know exactly what cycles of treatment we have to conduct in each case, and the doses that have to be used and the proportions between the different cannabinoids are not defined either.
Then, why do we use cannabinoids already?
Basically due to their low toxicity; we know their side effects that we mentioned in other articles, and we can handle them safely in combination with other drugs in most cases, without finding adverse reactions or side effects that prevent us from performing the treatment or that may jeopardise the stability of the patient.
Not all patients tolerate treatment in the same way, and its effectiveness is not the same in all cases. It should be noted that most patients start complementary treatment with cannabinoids in advanced phases of the process, so the results are very logically related to this fact. We can use THC without the patient reporting any limiting psychoactive effect, which is good news for patients who are logically concerned about this situation.
It is very important to consult a doctor if we are going to incorporate cannabinoids in a treatment in general, because we have to take into account contraindications, drug interactions, and evaluate the characteristics of each patient to indicate or not complementary treatment with cannabinoids.
We have to study the medical documentation of each case and obtain the necessary data to assess indication or not of treatment with cannabinoids.
The types of cancer that could be treated with cannabinoids would be glioblastomas, some types of breast cancer, colon cancer, lymphomas, leukaemia, prostate cancer, pancreatic cancer, lung cancer and gastric cancer.
Always insisting that most of the information comes from preclinical studies, and there are no conclusive proven results in humans.
It is never too late to talk a little about the true protagonist of this story, which is the Endocannabinoid System, since, with the cannabinoids of the plant we act through specific receptors and we obtain the effects that cannabinoids generate in us when we use them. The antitumour effects are also exercised through these receptors.
We use the Phyto cannabinoids, in this case, as modulators of the endocannabinoid system, but there are other molecules that can also act on these receptors, which are not the cannabinoids of the plant, and that is why we speak about "promiscuity" of this system, because different substances can interact with the receptors, and can alter the function of the endocannabinoid system, which is the most important and complex, and least studied, regulation system, humans have.
We must bear in mind that from a medical point of view, there are a multitude of clinical studies that tell us which cannabinoids are those indicated, a what dose they should be administered, and that cycles of treatment that must be met. Therefore, I am of the opinion that we lack even the necessary data for use cannabinoids as antitumour agents with guarantees.
Another issue is that, for the time being, cannabinoids are used together with chemotherapy agents, and to alleviate the symptoms that accompany cancer patients.
I respect in any case patients who choose treatment with cannabinoids as monotherapy, of course. It is a right to choose the treatment that looks like the best, after having been properly informed of the therapeutic alternatives in each particular case.
The toxic symptoms resulting from chemotherapy causes in most cases side effects that require in some cases specific medication.
Cancer patients usually report weight loss, accompanied by lack of appetite, as well as sleep disorders and mood disorders, which tends to be an anxiety depressive disorder, and pain in greater or lesser degree, in addition to nausea and vomiting secondary to chemotherapy. In this context cannabinoids are effective for treating these symptoms reported, and it is necessary to find the right combination and the exact therapeutic dose for each patient. To treat these symptoms, varieties with a 1/1 ratio, CBD/THC, are valid, but without forgetting that THC is important for most of the symptoms. Probably the use in this case of an extract rich in CBD without THC would possibly would not offer the same result, with a worse effect on appetite and the vomiting that accompanies chemotherapy in some patients. On the basis of tolerance to treatment, we have to use different ratios or proportions of THC/CBD with each patient, according to tolerance, basically to THC, in relation to their psychoactive effect.
We can already at the moment act in a controlled manner with 3 cannabinoids, THC, CBD and recently CBG. We have products on the market with CBD and CBG correctly analysed and tested. An analysis of the products to be used is essential to know the concentration of cannabinoids and be able to accurately dose. Doses are calculated in relation to the patient's weight. Other cannabinoids also interesting from a cancer point of view such as CBG, would be CBGV or Cannabigerovarin and THCV or Tetrahydrocannabivarin. They have the problem of accessibility, since they are in very low percentages in most varieties, at least from what we presently know. THCV is usually found in higher percentages in some South African and Thai Asian varieties. But of the 111 cannabinoids characterised today little is known in relation to their effects, metabolism and therapeutic potential. Much remains to be done with this family of interesting molecules of vegetable origin.
Cancer patients can benefit from treatment with cannabinoids to treat the symptoms resulting from chemotherapy and improve quality of life.
How can cancer patients handle cannabinoids?
First we must recommend medical supervision of treatment, especially if there is no prior experience in the use of cannabis. It is important to rule out contraindications and assess possible interactions of the treatment prescribed by the oncologist. Let us remember that use of cannabinoids is complementary to cancer treatment. We have no conclusive data as to advise treatment with cannabinoids as monotherapy or single therapy.
We have to differentiate palliative use of cannabinoids, which would aim to control or improve the symptoms that the patient presents from use with an antitumour purpose, which many patients seek, as they have accessed information indicating that "high" doses of cannabinoids, above all THC, can "cure" cancer. Currently we do not know exactly what dose we have to use, which cannabinoids we have to use and how long we have to use them for, for the 200 different types of cancer recognised by the WHO.
Cancer patients can at least improve their quality of life in many cases, and in others they can have very positive results on the evolution of the disease, but scientifically we cannot present any conclusive and reliable results, among other factors, due to the great diversity in the types of cancer, and in most cases, the patient when he/she visits is already in advanced stages of the disease, and it is essential to act as soon as possible, obviously. Cancer treatments such as chemotherapy and radiation therapy are more effective with complementary treatment with cannabinoids in many cases, and the patient tolerates much better the side effects of treatment, as well as nausea and vomiting, loss of appetite, sleep disorders, mood, pain. Very frequent symptoms in cancer patients.
The most used route of administration would be the sublingual route, using oils or tinctures which gives us more stable absorption than in the oral route. In cases where we are treating a type of brain cancer, this is the route of choice, as we manage to save the first hepatic metabolic step of the THC, and it directly passes the blood-brain barrier to be distributed directly by the brain tissue.
The effect can take between twenty minutes and one hour to appear, depending on the characteristics of each patient, although in half an hour most patients already detect the effect.
The oral route is going to determine a more irregular absorption, and the effect can take between half an hour and an hour and a half to appear, but it is a practical route, and when we have been receiving treatment for a few days, we can maintain an acceptable mean absorption that allows us to maintain the effect in a stable manner.
Vaporisation of whole plant is a very interesting resort as it provides us with an almost immediate effect. In addition, if the plant is analysed we can, when we weight it, prepare the doses with acceptable accuracy. A patient who is undergoing treatment with THC and CBD, orally, for example, can vaporise as a salvage therapy on demand, since, on noticing the effect quickly, he/she can dose depending on if he/she needs more or less effect. But for non-smokers, it is more difficult to use it correctly, because although you inhale steam and not smoke, the steam must reach the lung alveoli, for the cannabinoids to be properly absorbed.
Today, we can vaporise also extracts or concentrates of cannabis, and it is very important to reflect on the percentages of cannabinoids that we find in these extracts, especially in the different types of BHO.
We handle 80% of percentages of THC, which tells us that in 100 mg of extract we have 80 mg of THC. We must be very careful with the dose if we use these extracts, since they contain a large amount of THC. From here the anecdote of the "grain of rice" that has left more than one patient knocked cold who had no previous experience with cannabis. We have to know what quantities we are using.
We know that chronic cannabis users require increasingly higher doses of THC to get the same effect. We refer to this phenomenon as tolerance. CBD does not seem to generate the same problem, because in clinical practice, maintained doses generate the same effect without the need to increase them. Patients who have used cannabis previously know its effects and may have had positive experiences or not, so we have to take special care with patients who have had bad experiences with cannabis and the psychoactive effect. In chronic users it is very difficult to dose because tolerance to THC is generated due to its continued use.
The patient should tolerate the treatment well, not presenting psychoactive effect and generating an area of comfort that reasonably meets his/her expectations according to the pathology we are dealing with. In our clinical experience, the use of CBD allows us to work with THC also, without the patient present a limiting or unpleasant psychoactive effect. Not all patients tolerate cannabinoids in the same way, we have to correct the THC/CBD ratios and the doses, to adapt each patient to the treatment.
If we work with ratios close to 1/1 (THC/CBD) we minimise the psychoactive effect of THC; if we increase THC, the psychoactive effect is increased on exceeding the amount of CBD. The Indica varieties, given their composition in terpenes and cannabinoids, usually provide a relaxing corporal effect, with hypnotic and analgesic properties that can induce sleep, so their use is advisable in the evening doses. We find myrcene above 0.5% as the main terpene in most Indica varieties, which enhances these effects.
The Sativa varieties in general will provide us with a more cerebral, euphoric, analgesic effect, and usually do not induce sleep, which makes them more useful during the day if the patient has to perform physical tasks. We find terpenes such as borneol, uncommon in Indica varieties.
It is interesting to take the origin of cannabinoids into account when we work with extracts or dilutions of a whole plant, because the same doses of THC will have different effects depending on the extract or the dilution of Sativa or Indica source.
Sources consulted / SEIC / IACM / PubMed / GH Medical.