By Eduardo Muñoz

Doctor in Medicine and Surgery, Professor of Immunology at the Department of Cellular Biology, Physiology and Immunology of the University of Cordoba and Director of the Inflammation and Cancer Research Group at the Maimónides Institute of Biomedical Research in Cordoba. Dr Muñoz Blanco’s research centres on the study of cannabinoids in inflammatory diseases and the development of new semi-synthetic cannabinoids. In 2003, he founded VivaCell Biotechnology España, which develops new pharmaceuticals based on non-psychotropic cannabinoids.
The skin is the largest organ in the human body. One of its principal functions is to protect the body against external agents and it is the first defensive barrier of the innate immune system. Other important functions of the skin include controlling body temperature, maintaining the hydro-electrolytic balance and perceiving painful or pleasurable stimuli. Any alteration in the functioning or appearance of the skin can have important consequences for our physical and mental health. Many of the problems that present in the skin are limited to it. In some cases, however, the skin can reveal a disorder affecting the entire body.
Development of Pharmaceuticals in Dermatology
Nearly 37% of primary health care patients have some acute or chronic skin disease and it is surprising how few new pharmaceuticals are being developed to treat these conditions –particularly those most commonly treated by dermatologists and non-dermatologists– when compared to other pathologies. One important reason why few pharmaceutical companies are developing drugs for skin diseases is that the economic return on such drugs (especially topical skin products) is relatively small when compared to the market for pharmaceuticals for other conditions (e.g. cardiovascular diseases) (Eaglstein and Corcoran, 2011).
Another factor limiting the development of pharmaceuticals based on natural products –including preparations of Cannabis sativa– is the fact that in most cases it is not possible to establish adequate protection for intellectual property of the drug, an essential inventive to investment in the development of new pharmaceuticals for any application. It is therefore hardly surprising that the great majority of skin diseases, especially inflammatory diseases, are treated with over-the-counter health-care (para-pharmaceutical) products whose effectiveness, in most cases, is not proven.
Cannabinoids in Dermatology
The topical use of Cannabis sativa L dates back to ancient China, where cannabis preparations were used externally to treat skin rashes, ulcers, wounds and hair loss. There is also archaeological evidence suggesting that topical cannabis preparations were used by the ancient Egyptians to treat eye conditions and also in bandages for wounds. Cannabis leaves were used in medieval Arab medicine to treat skin diseases such as pityriasis and lichen planus. More recently, in the early twentieth century, before prohibition, tinctures of cannabis were commonly sold in pharmacies. Among other applications, they were used to treat calluses, irritable bladder, menstrual pains and as an aid for quitting opium addiction.
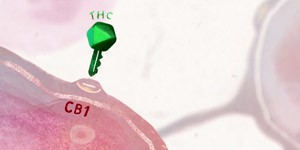
The skin possesses all the elements of the endocannabinoid system, i.e., endocannabinoid compounds (AEA and 2-AG), metabotropic (CB1R and CB2R) and ionotropic (TRPV-1) receptors of cannabinoids and the enzymes involved in the synthesis and metabolism of endocannabinoids (e.g. FAAH and MAGL). The various elements in the endocannabinoid system are involved in key mechanisms of skin regulation, such as control of growth of the epidermis and skin annexes, cell survival, immune and inflammatory responses, the transmission of sensory stimuli to the central nervous system (pain, itching) and the synthesis of lipids, among other activities.
Despite this long history of topical use of cannabis and advances in our understanding of the endocannabinoid system of the skin, research into the use of cannabinoids for skin pathologies is one of the youngest fields of research in this area and clinical data on the use of cannabis in dermatological practice remain extremely limited. Nonetheless, there is increasing evidence of the potential of cannabinoids for the treatment of inflammatory skin diseases, including psoriasis and atopic dermatitis and for the treatment of auto-immune diseases such as scleroderma, characterised by inflammation and fibrosis.
Psoriasis
Psoriasis is one of the most common chronic inflammatory skin diseases. It is characterised by hyper-proliferation and shedding of keratinocytes, resulting from infiltration of T-cells and neutrophils and activation of dendritic cells and macrophages. Although the pathogenesis of psoriasis is not fully understood, there is solid evidence to suggest that deregulation of the immune cells in the skin, in particular Th1 and Th17 cells, plays a critical role in the development of psoriasis.
Although there is at present only anecdotal evidence on the use of Cannabis sativa L preparations for topical use in psoriasis, the therapeutic possibilities of cannabinoids acting through CB2R and through mechanisms that are independent of classical cannabinoid receptors are very broad given their role in the regulation of Th1 and Th17 lymphocytes (Derakhshan and Kazemi, 2016). It has also been seen that some phytocannabinoids inhibit the proliferation of keratinocytes through non CB1R and CB2R paths (Wilkinson and Williamson, 2007).
Atopic dermatitis
Atopic dermatitis (AD) is the most frequent chronic inflammatory disease of the skin. Initiation and progression of the disease are induced by interactions of genetic, environmental and immunological factors. The clinical characteristics of AD include dryness of the skin through loss of the epidermal barrier, erythema, exudation, scabs and lichenification. Moreover AD is characterised by intense itching which leads to frequent scratching and infection by staphylococcus. There is no cure for AD and the main goals of treatment are to reduce the symptoms (itching and dermatitis), prevent exacerbations and minimise the risk of skin infection. Standard forms of treatment for managing AD patients centre on the use of anti-inflammatory topical preparations with corticoids and hydration of the skin, but in serious cases, patients may require systemic treatment with powerful immunosuppressives –such as cyclosporin A or tacrolimus– and antibiotics to prevent infection by staphylococcus-type bacteria.
Numerous para-pharmaceutical preparations are now available based on oil from Cannabis sativa L seeds, especially hemp, for the treatment of AD. However, despite the misleading advertising often used to market such products, hemp seed oil does not contain cannabinoids or other bioactive phenolic compounds, and its therapeutic effect goes no further than any other preparation containing polyunsaturated fatty acids and favouring skin hydration.
However, to judge from pre-clinical studies, cannabinoids also have great potential for therapeutic management of AD (Ong PY, 2009; Wollenberg and cols, 2014). In this regard, selective CB1R agonists inhibit the activation of mastocytes and the release of histamine. Moreover, topical application of anandamide analogs has been shown to reduce skin inflammation in animal models of AD (Kim et al., 2015). Other authors have suggested that CB1R expression in keratinocytes plays a relevant role in maintaining the epidermal barrier (Gaffal et al., 2014). Finally it has also been described that the release of histamine from CB2R inhibits the inflammatory skin reaction mediated by IgE and intense spontaneous pruritus in AD (Maekawa et al., 2006).
The antibacterial action of Cannabis sativa preparations and phytocannabinoids has been well known for decades, although only more recently has the antibacterial activity of cannabinoids THC, CBD, CBG and their precursors (acid forms) against methicillin-resistant staphylococcus been demonstrated (Appendino et al., 2008).
Nearly 100 cannabinoids have been identified in the plant, together with a large number of other bioactive compounds, such as phenolics and terpenes, which also have important antioxidant and anti-inflammatory activities (Hanuš et al., 2016; Russo, 2011). The cannabinoids and other types of compound are thought to have interacting synergic effects. This would explain why in some in vitro studies, better results have been obtained with extracts from the plant than with pure isolated compounds. Although the content of cannabinoids and other types of compound varies depending on the variety of plant, cannabinoids can be said to have huge potential for treating AD, given their anti-inflammatory and antibacterial properties.
Cannabinoids and fibrotic skin diseases
Systemic scleroderma (or sclerosis) (SSc) is a rare autoimmune disease that has three main characteristics: dysfunction of fibroblasts, leading to an increase in the deposition of proteins from the extracellular matrix, vasculopathy of small vessels resulting in tissue hypoxia and an immune response with production of proinflammatory cytokines and autoantibodies. SSc is characterised by progressive thickening and fibrosis of the skin, secondary to excessive accumulation of collagen, which can be limited to the skin (localised –or limited– cutaneous SSc) or extend to internal bodies (diffuse SSc). SSc begins with a microvascular injury and inflammation. This is followed by fibroblast activation, a key event in the development of fibrosis.
Recent evidence shows that genetic and pharmacological manipulation of the endocannabinoid system modulates the fibrotic response. CB1 and CB2 receptors, too, have shown different patterns in experimental models of dermal fibrosis. Blockage of CB1R prevents activation of fibroblasts and has a powerful antifibrotic effect (Marquart et al., 2010). The role of CB1R as a profibrotic receptor has also been confirmed in knock-out mice for FAAH, in which high levels of endocannabinoids can induce fibrosis through a CB1R-dependent path. On the other hand, activation of CB2R prevents cutaneous fibrosis and the infiltration of tissue leukocytes in models of experimental dermal fibrosis (Akhmetshina et al., 2009). As a result, JWH-133, a synthetic agonist of CB2R abrogates experimental dermal fibrosis in mouse models. This concurs with the fact that the CB2R knock-out mice are more susceptible to the development of fibrosis (Balistreri et al., 2011). It has also been demonstrated that PPARγ agonists inhibit the profibrotic response by inhibiting the TGFβ signalling path. It has also been demonstrated that dual agonists of PPARγ/CB2R show a powerful anti-inflammatory and anti-fibrotic activity in experimental models of SSc (Del Río et al., 2016).
References:
1. Akhmetshina, A. Dees C, Busch N, Beer J, Sarter K y cols. The cannabinoid receptor CB2 exerts antifibrotic effects in experimental dermal fibrosis. Arthritis and rheumatism 2009; 60:1129-1136.
2. Appendino G, Gibbons S, Giana A, Pagani A, y cols. Antibacterial cannabinoids from Cannabis sativa: a structure-activity study. J Nat Prod. 2008; 71:1427-30.
3. Balistreri E, Garcia-Gonzalez E, Selvi E, Akhmetshina A, y cols. The cannabinoid WIN55, 212-2 abrogates dermal fibrosis in scleroderma bleomycin model. Annals of the rheumatic diseases 2011; 70: 695-699.
4. Derakhshan N, Kazemi M. Cannabis for Refractory Psoriasis-High Hopes for a Novel Treatment and a Literature Review. Curr Clin Pharmacol. 2016; 11:146-7.
5. del Río C, Navarrete C, Collado JA, Bellido ML y cols. The cannabinoid quinol VCE-004.8 alleviates bleomycin-induced scleroderma and exerts potent antifibrotic effects through peroxisome proliferator-activated receptor-γand CB2 pathways. Sci Rep. 2016:18; 6:21703
6. Di Marzo V, Bifulco M, De Petrocellis L. The endocannabinoid system and its therapeutic exploitation. Nat Rev Drug Discov. 2004; 3:771–784.
7. Eaglstein WH, Corcoran G. New drugs and new molecular entities in dermatology. Arch Dermatol. 2011 May;147(5):568-72.
8. Gaffal E, Glodde N, Jakobs M, Bald T y cols. Cannabinoid 1 receptors in keratinocytes attenuate fluorescein isothiocyanate-induced mouse atopic-like dermatitis. Exp Dermatol. 2014; 23:401-6.
9. Hanuš LO, Meyer SM, Muñoz E, Taglialatela-Scafati O, Appendino G. Phytocannabinoids: a unified critical inventory. Nat Prod Rep. 2016. 33:1357-1392.
10. Iannotti FA, Hill CL, Leo A, Alhusaini A y cols. Nonpsychotropic plant cannabinoids, cannabidivarin (CBDV) and cannabidiol (CBD), activate and desensitize transient receptor potential vanilloid 1 (TRPV1) channels in vitro: potential for the treatment of neuronal hyperexcitability. ACS Chem Neurosci. 2014; 19:1131-41.
11. Kim HJ, Kim B, Park BM, Jeon JE y cols. Topical cannabinoid receptor 1 agonist attenuates the cutaneous inflammatory responses in oxazolone-induced atopic dermatitis model. Int J Dermatol. 2015; 54:e401-8.
12. Maekawa T, Nojima H, Kuraishi Y, Aisaka K. The cannabinoid CB2 receptor inverse agonist JTE-907 suppresses spontaneous itch-associated responses of NC mice, a model of atopic dermatitis. Eur J Pharmacol. 2006; 542:179-83.
13. Marquart S, Zerr P, Akhmetshina A, Palumbo K y cols. Inactivation of the cannabinoid receptor CB1 prevents leukocyte infiltration and experimental fibrosis. Arthritis Rheum. 2010; 62:3467-76.
14. Ong PY. Emerging drugs for atopic dermatitis. Expert Opin Emerg Drugs. 2009; 14:165-79.
15. Russo EB. Taming THC: potential cannabis synergy and phytocannabinoid-terpenoid entourage effects. Br J Pharmacol. 2011. 163:1344-64.
16. Sido JM, Nagarkatti PS, Nagarkatti M. Role of Endocannabinoid Activation of Peripheral CB1 Receptors in the Regulation of Autoimmune Disease. Int Rev Immunol. 2015; 34:403-14.
17. Turcotte C, Blanchet MR, Laviolette M, Flamand N. The CB(2) receptor and its role as a regulator of inflammation. Cell Mol Life Sci. 2016; 73: 4449-4470.
18. Wilkinson JD, Williamson EM. Cannabinoids inhibit human keratinocyte proliferation through a non-CB1/CB2 mechanism and have a potential therapeutic value in the treatment of psoriasis. J Dermatol Sci. 2007; 45:87-92.
19. Wollenberg A, Seba A, Antal AS. Immunological and molecular targets of atopic dermatitis treatment. Br J Dermatol. 2014; 170 Suppl 1:7-11.