By Manuel Guzmán

Manuel Guzmán is Professor of Biochemistry and Molecular Biology at Complutense University of Madrid, member of the Spanish Royal Academy of Pharmacy, and member of the Board of Directors of the International Association for Cannabinoid Medicines. His research focuses on the study of the mechanism of action and therapeutic properties of cannabinoids, especially in the nervous system. This work has given rise to more than one hundred publications in specialized international journals, as well as to several international patents on the possible therapeutic applications of cannabinoids as anticancer and neuroprotective drugs. He routinely collaborates with scientific reviewing and funding agencies.
The vast majority of clinical studies that support the therapeutic use of what is usually known as "cannabis" have actually been carried out with purified cannabinoids (especially the THC phytocannabinoid and its synthetic derivative nabilone), as well as with a standardised extract of Cannabis sativa that contains an equimolecular proportion of THC and CBD (Sativex). Unfortunately, and largely due to the prohibitionist regulations that have been in place for decades worldwide, very few studies have contemplated the use of, for example, vaporised herbal cannabis or cannabis oils. With the information available these days, what can be suggested or interpreted about how similar or different the therapeutic effects are of these types of preparations that are so varied?
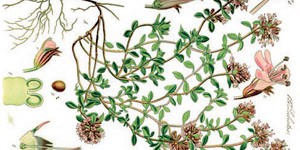
Cannabis is a very heterogeneous substance from the chemical point of view and therefore it is not easy to define its precise effects on a specific user. Each patient is an individual biological entity and, for example, a strain of cannabis (or a certain dose of it) that is appropriate for one individual may not be suitable for another. Considering the hundreds of compounds detected so far in C. sativa preparations (cannabinoids, terpenes, polyphenols, steroids, flavonoids, etc.), it is clear that a substantial part of them can, at least theoretically speaking, exercise biodynamic actions on the human organism. In fact, there are no accurate scientific studies on the effects of the vast majority of these compounds and not to mention their possible biochemical interactions. However, it is very well accepted today that the pharmacological properties of cannabis (in mice and in other experimental animals as well as in Homo sapiens) are essentially due to cannabinoids, of which we already know a great deal about. Although C. sativa produces these compounds in carboxylated form (e.g. THCA and CBDA), the vast majority of the therapeutic use of cannabis and cannabinoids has so far been restricted to decarboxylated forms, which mostly contain THC and/or CBD, and therefore are those considered in this article.
Based on studies carried out in cells and experimental animals, some pharmacological interactions have been described between different components of cannabis, for example in regard to its hepatic metabolism action by enzymes of the CYP family. However, there is still no scientific/clinical evidence that such interactions occur significantly in real medicinal cannabis users. In my opinion, in fact, it seems very likely that the famous "entourage effect" has been over interpreted in its original sense (for example, endogenous molecules similar to anandamine facilitate its biological activity) as well as in its extrapolation to cannabis (for example, terpenes and cannabinoids other than THC facilitate its therapeutic activity). Thus, the "classical" therapeutic properties of THC-rich cannabis preparations are conceivably due to THC activating the CB1 cannabinoid receptor in precise anatomical locations of the human organism. This includes, for example, inhibiting nausea and vomiting, stimulating the appetite, attenuating energy expenditure, reducing spasticity and reducing pain (in this latter case, it is also likely that effects mediated by the CB2 cannabinoid receptor are involved). On the other hand, the therapeutic properties of cannabis preparations rich in CBD are conceivably due to the biodynamic action of CBD (whose molecular bases are not yet known in detail). This includes, for example, the anticonvulsant and antipsychotic effects exerted by this compound. CBD has recently become a "new media molecule" or "magic pill", to my way of thinking in an erroneous way to become this notion based essentially on over interpretation of laboratory studies; read as, "if it works in mice it will work in patients." It is easy to understand that this reasoning is incorrect and, in fact, we still have a lot to learn about the effects of CBD in human beings, not only in the aforementioned and more advanced fields of epilepsy and schizophrenia, but in other possible niches such as ulcerative colitis, graft-versus-host disease, anxiety disorders and metabolic diseases, to name a few in which promising studies are currently underway.
In any case, the notion that CBD can increase the safety of cannabis preparations is increasingly accepted, so that balanced preparations between THC and CBD would have a greater therapeutic window than preparations rich in THC and poor in CBD. The latter can cause, for example, acute episodes of psychosis and anxiety. However, a question still without a precise answer is 'what are the best THC/CBD ratios for each disease and particularly the pathological stage?' Addressing this problem would require a huge research effort in the laboratory and, especially, in clinical studies. In my opinion, the impact of these studies on specific variables in the large populations of patients required would be predictably small. Therefore, in practical terms, I believe that it is necessary to "customise" this aspect and define the THC/CBD ratios that are best adapted (in terms of efficacy and tolerability) to the specific needs of each specific patient at each specific moment. So far, for large cohorts of patients, there are only rigorous studies with Sativex, whose initial clinical data soon converged to a THC/CBD "commitment" ratio of 1:1. For the "classic" therapeutic cannabinoid applications, especially spasticity and neuropathic and oncological pain as the most studied with Sativex, the average maintenance dose is about 8 sprays (= 22 mg of THC and 20 mg of CBD) per day. Unfortunately, there are still no analogous data with standardised cannabis extracts containing other THC/CBD ratios.
As for terpenes, there is currently no precise knowledge about their biological actions or pharmacological interactions with cannabinoids in the human organism. It is possible that certain terpenes may facilitate some of the therapeutic actions of cannabinoids (e.g. β-caryophyllene anti-inflammatory action and myrcene sedative action). However, also bear in mind that some terpenes could have adverse effects on the health (for example, limonene and linalool generate dermal allergens by oxidation, as well as methacrolein, benzene and other toxic products by combustion). In summary, deeper studies are also undoubtedly required in this field.
Another question that sometimes arises is the use of cannabinoids isolated from cannabis compared with cannabinoids synthesised in the laboratory. It is clear that for an individual phytocannabinoid there should not be any chemical difference; for example, pure Δ9-THC is a unique molecular entity, with the same atomic composition and stereochemistry regardless of whether it is obtained from cannabis or produced in a laboratory. However, there may be differences between isolated cannabinoids from natural sources and those obtained in a laboratory if the chemical synthesis process is not carried out correctly and side reaction products or other impurities are generated during it. For example, there is data that two stereoisomers of CBD, denoted as (+)-CBD and (-)-CBD, have different biodynamic properties, so if mixtures of both the resulting overall product are obtained in a synthesis process it may have barely predictable pharmacological action and different from that of the (-)-CBD present in cannabis. In short, in vitro cannabinoids must be synthesised in a very precise way to generate a product that can be traced correctly. Regarding the synthetic phytocannabinoid derivatives, despite the many efforts made over the past three decades by numerous laboratories around the world, only nabilone has reached the market so far, and its pharmacological characteristics (high receptor activating power) CB1 cannabinoid, erratic digestive absorption, narrow therapeutic window, etc.) have not allowed it to become a valid therapeutic alternative to THC/dronabinol, Sativex or standardised cannabis preparations. So today, in the medicinal field, we must essentially stick to the use of phytocannabinoids or cannabis preparations and not synthetic cannabinoids.
In short, cannabis is a plant with a complex and varied chemical composition, so it is essential to define its precise chemotype(s) in order to offer it to a specific patient as a more valid therapeutic option. However, roughly speaking, THC is the main therapeutic agent in the most commonly used cannabis preparations; that is, those that have high THC/CBD ratios, while CBD is in some less common cannabis preparations that have high CBD/THC ratios. The presence of CBD can provide greater safety and thus expand the therapeutic window of THC. In other words, a combination of THC and CBD, or a cannabis preparation rich in THC and CBD, obviously if well standardised and traced, could be considered a "therapeutically improved version of THC". However, I believe that it is still not possible to firmly support the existence of an "entourage effect" in cannabis beyond this possible complementary action between THC and CBD, its two main cannabinoids. Unfortunately, it is impossible to conceive clinical trials today with tens of thousands of patients to compare different pure cannabinoids, either alone or in combination with other cannabinoids and terpenes, together with cannabis extracts, administered by different methods and for different diseases. This is absolutely beyond our reach in economic, human and temporal terms, especially under the current restrictive regulatory frameworks for conducting clinical studies with substances considered to be narcotic drugs. Therefore, in more realistic terms, a multifactorial approach to the problem could be considered from three complementary levels: (a) Preclinical studies (in cells in culture and laboratory animals) aimed at researching interactions between different compounds (cannabinoids and non-cannabinoids) from a biochemical, pharmacological and behavioural perspective could suggest candidate combinations for use in therapy. (b) Controlled clinical trials with the most appropriate selection of such combinations of compounds could provide accurate data on efficacy and safety (e.g. dosage and treatment durations, pharmacokinetic parameters). (c) Observational studies with different chemotypes, preparations and administration methods, mainly under the umbrella of medicinal cannabis dispensing programmes, could provide information about whether, for example, cannabis oils or herbal cannabis are more effective and/or better tolerated than THC and CBD (alone or combined in different proportions).