By Raquel Peyraube

Dr. Raquel Peyraube is a doctor in medicine and a specialist in the problematic use of drugs. She has trained in psychiatry, toxicology and psychoanalytical psychotherapy and in subjects such as childhood, adolescence and social exclusion. She has 28 years' experience in the field. Throughout her career, she has made contributions in training, prevention, treatment and damage reduction, including innovating theoretical and methodological developments with emphasis on ethical issues. As a former clinical director of ICEERS, she is now an ad hoc consultant of the Uruguayan National Drugs Secretariat giving advice on reform of the public drugs policy and of the Institute of Cannabis Regulation and Control. She is a clinical researcher and a member of research teams for monitoring the law in Uruguay. She sits on several international scientific committees and is an active member of the IACM (International Association for Cannabinoid Medicines). She currently works on the development of clinical trials, medical education on medicinal cannabis, and dissemination of information and advice for reform of drugs policies in various countries.
As more and more information becomes available on the potential benefits of using cannabinoids for certain ailments, increasing numbers of people are trying to seek out such treatment. Some consult their treating physician about the possibility; others, afraid of their doctors’ reaction, start using cannabis-based products under the guidance of suppliers or based on information they find on different websites, not all of which provide thorough and accurate information.
For this reason, I would like to share my approach to conducting such consultations at my practice with any of my colleagues wishing to offer their patients guidance in this course of action. Whether or not they have decided to dedicate themselves to this specialist area or conduct this type of treatment, GPs and consultants are important figures for patients and their support and mentoring can have a beneficial practical and psychological effect in the decision-making process.
I also hope to offer information that will enable patients wishing to consult their doctors to prepare for that meeting. For physicians who are unfamiliar with such treatments or have doubts as to their safety and effectiveness, seeing a responsible attitude among patients can make the difference in the way they respond.
The scientific bases for these treatments are dealt with exhaustively in the literature and I shall not discuss them here; at the end of this article, you will find a recommended reading list. I will simply comment on my own practice and aspects on which there is consensus among those of my colleagues who are approaching this practice in a serious and rigorous fashion. The basic outline of the consultation is similar to that used for any other conventional form of medicine – which is exactly what cannabis medicine is. The one difference lies with certain subjective aspects and issues related to the patient's education, which have heretofore been ignored in clinical practice, as well as other aspects arising from the current state of the art of cannabis medicine. For each of the items listed, you will find remarks aimed at physicians and patients.
1. Reason for consultation (new patient): Diagnosis and treatments
1.a. Physicians: You should start by finding out more about the condition on which the patient is consulting. It is important to find out about any previous treatment and any medication the patient is currently taking, in order to determine what results have been achieved with these treatments and assess potential interactions with cannabinoids.
1.b. Patients: Bring along any relevant information about your condition and the medication you are receiving to the consultation. It may be helpful to bring a summary of your clinical record (your doctor can prepare this) with a list of medicines you are currently taking and the dose.
2. Why cannabis? What led the patient to consider this possibility?
2.a. Physicians: It is important to find out why the patient is considering this type of treatment. Bear in mind that many patients will have made their own enquiries and know of other cases with the same or other pathologies that have yielded good results. Others have no prior information at all, while others come out of desperation, with little-understood ailments for which there is no effective treatment – and for which cannabinoid research offers no solutions either. If this is the case, you should tell them so. In such cases, the patients’ goal is sometimes just to try to relieve some of their symptoms and improve their quality of life. This is an entirely valid objective, since this is exactly what cannabis medicine can offer.
2.b. Patients: However much you may or may not know about these treatments, we recommend that you be quite clear about your reasons for seeking them and that you take a serious and responsible approach to this alternative.
If you have made up your mind to follow this course of action, it would also be helpful if you shared your decision with your treating physician and asked him or her for assistance in your search. If your GP or consultant admits to not knowing much about the subject, you can offer to keep them informed and put them in contact with the professional who will be conducting the cannabinoid treatment. You can also contribute by furnishing reputable scientific sources of information such as the reading list provided at the end of this article.
If your physician rejects treatment, not on the basis that such treatment is not indicated for your condition, but on the grounds of beliefs and moral values, you should tell him or her that you intend to look for another doctor to guide you. Patients have a right to a second opinion.
3. Prior and present experience with cannabis? (Recreational and/or medicinal use)
3.a. Physicians: You should try to determine whether the patient has already tried cannabis –for recreational or medicinal purposes– and whether they are currently consuming it. Ask what products they use, their composition, origin, results and any adverse effects. Patients have often already tried cannabis under the guidance of suppliers or following recommendations they have found on the Internet, but do not feel safe without medical guidance. In some jurisdictions there are patients’ associations with accumulated experience and training which can provide information and support. Nonetheless, patients generally prefer to have medical guidance.
As for any adverse effects (see cuadro 1), depending on their nature and intensity, they may not necessarily contraindicate the use of cannabis. They may be caused by the specific products being used, incorrect dosage or failure to take into account interactions with other drugs.
3.b. Patients: It is essential that you be fully transparent and honest with the doctor in order to build up the necessary relationship of trust and make sure your doctor has all the necessary information. If you’re already using these products or have used them in the past for non-medical purposes, it is important that you tell your doctor about your experience: Any wanted and unwanted effects, “bad trips” (in recreational use) or other adverse effects.
4. Education of patients and their close relations:
4.a. Physicians: Depending on the legal context regarding the use of cannabis and cannabinoids, and even if they have made up their minds to try these treatments, patients and their relatives may have prejudices and fears in this regard. They may also have heard positive or negative ‘legends’ about these treatments which they take at face value. As with any treatment, mistrust and fear (the set) may influence in adverse effects. A secure context and good preparation (the setting) also impact the results. Understanding the reason for the medical indications increases patient adherence and helps promote a responsible attitude.
Any unrealistic expectations or hopes of a cure that the patients may bring to the treatment should be dealt with. We are not shamans; we are doctors and in general we cure very few diseases. Until the scientific evidence proves otherwise, we should not speak of curing but of improving, relieving and alleviating. Patients should be told that in the event of a favourable response, the best results they notice will be related to their quality of life and improvements in certain symptoms; however, we do not know whether it is possible to influence the development of the disease. They should be warned that not all cases have a positive response.
With the right education on the endocannabinoid system (eCS), you can improve many of the issues discussed above. Regardless of what you may think of cannabis and cannabinoids, it is your responsibility as a doctor to understand the eCS. This is a vitally important physiological system in the body whose presence has been known of for over 20 years. If you don’t know about it, it’s time you learned – and prepared for receiving consultations of this kind. We should not still be hearing the words “I don't believe in that” from a certain sector of doctors. This is not some religion or god to be believed in or not. It is scientific evidence.
Patients readily understand that, just as when the endocrine system fails, we provide hormone replacement treatments (e.g. with thyroid hormone or insulin), we can also provide plant-produced cannabinoids when their eCS is deficient or uncontrolled.
This part of the consultation may take quite a long time and you may sometimes need to schedule two separate appointments. In order to optimise the time, some health centres and doctors working in this area prepare information material which patients can read before coming to the consultation.
4.b. Patients: You should honestly consider your real expectations and separate them from what you would like to happen. There are plenty of stories doing the rounds about cures, but none of them have been scientifically validated. That does not mean they are not possible, simply that we cannot be sure that the apparent cure is due to the action of the cannabinoids.
We recommend that you go to the interview prepared to take notes. It will not be easy to take in all the information during the consultation. You can go back to your notes later to clear up any queries you have and make any decisions. Don’t feel embarrassed to ask anything you need to know until you are quite sure about all aspects, even if you think your questions might seem trivial.
5. Family and personal antecedents – general ailments and mental health
5.a. Physicians: This information is particularly important when you are deciding on the recommended type of cannabinoid and dose; it will help avoid possible adverse effects that might present in patients with psychotic disorders or depression. Personal antecedents may show other conditions apart from the one the patient is consulting on. These conditions may also benefit from the treatment, a factor which should be assessed during the interview. Patients quite often report benefits not only in the condition for which they sought treatment, but others as well.
Personal antecedents of mental health pathologies should not be seen as an absolute contraindication for cannabinoid use; rather, they should determine the type of cannabinoid indicated.
5.b. Patients: When preparing for your consultation with the physician, it is important to take time to remember any diseases you or your next of kin may have had in the past, especially any related to mental health. It will not help to withhold information on such conditions out of a fear that you will not be prescribed or recommended treatment with cannabinoids. It might complicate the treatment and make it necessary to suspend it in the future.
6. Dosage, routes of administration and compounds
6.a. Physicians: The most realistic and feasible objectives of these treatments are to improve quality of life and certain symptoms of the condition about which the patient is consulting. It is therefore difficult to speak of compounds in jurisdictions where these products have not been legalised and regulated. Although we now know that there are other components as well as THC (psychoactive) and CBD (non psychoactive) which could have medical uses, at present all treatments are essentially conducted with THC and/or CBD.
At the same time, along with the products derived from the cannabis plant we also need to consider terpenoids, which can have an effect too. Please check the reading list for more information. However, in view of the current situation in most countries, there is a lack of quality control; this makes it difficult to guarantee natural products of a pharmaceutical quality with a known composition and cannabinoid concentration. The oils that patients acquire through different means –or prepare themselves– are uncertain. Naturally, this is not an ideal situation. Our aspiration must be to have products with different formulations suitable for different diseases and clinical conditions so that we can determine the profile of cannabinoids and terpenoids, the most suitable doses and routes of administration and ascertain whether they contain contaminants such as pesticides, heavy metals, solvents and aflatoxins. Fundación CANNA offers patients and doctors an analysis service to determine the composition and contaminant content of any products used.
Across much of the world, practitioners wishing to help their patients can avail of ‘compassionate use’, an option which allows patients to bring products into the country that are not registered in the official national pharmacopoeia, when the results of conventional treatments have proved unsatisfactory.
This is not the place to discuss the exact doses for each condition; moreover, the lack of clinical trials and uncertainty about composition make it impossible to offer any precise guidelines in this regard. The patients’ own experience can play an important part; they can report any positive or adverse effects and guide you in your recommendations. You should always start with sub-therapeutic doses and increase them slowly by small increments. The aim is to find the point of greatest benefit without causing adverse effects. You should tell the patient that this is how you are going to go about the treatment and ask them to be patient. An excessive increase might make it necessary to interrupt treatment, in order to flush out the cannabinoids before restarting treatment.
It is useful to have different routes of administration, to adapt to different clinical needs: fast-acting options, which will achieve quick but short-lasting peaks of plasma concentration, more prolonged routes, locally-acting products, etc.
6.b. Patients: We could repeat the same advice as for doctors; you must be patient if you want to avoid unwanted effects. You should understand that this is not some magic cure that will have sudden or magical effects. In addition, it does not always work for everyone and at all times. You should take great caution with what you consume and as far as possible test any products you have acquired (with composition and concentration analyses). If you would like more information on our service, please go to the Fundación CANNA website (http://www.fundacion-canna.es/en/types-of-tests)
7. Monitoring
7.a Physicians: For all of the reasons given above, together with the frequent possibility that the desired effects may vary throughout treatment, making it necessary to raise or lower the dose constantly, it is hugely important to monitor treatment. Given that we are working with an unbalanced control system, such changes in effectiveness are easy to understand. You also need to assess the presentation of certain effects caused by pharmacological interaction with other medicines the patient may be taking. These can generally be resolved by reducing the dose of the cannabinoids or other drugs. Physician and patient should work together in partnership; doctors need to listen to their patients who can often orient their recommendations.
7.b. Patients: People often talk about the wisdom of nature as a safe context for medical use of the cannabis plant. However, it is important to understand that most conditions that can be treated with cannabinoids are serious and patients are often receiving other medications that need to be adjusted depending on how the treatment develops. Monitoring is important and these treatments should not be trivialised – for good or ill.
You should be in no hurry to give up any conventional medication you are taking. It is not unusual for a sudden interruption like this to have a negative effect.
8. What conditions?
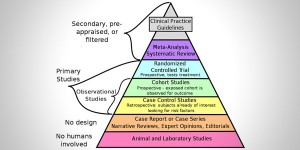
A short table is provided below of the potential uses of cannabinoids and cannabis. However, it is important to bear in mind that the evidence of the efficacy of cannabis medication varies between different conditions. Remember that there are very few clinical trials that provide secure and effective information on these treatments. For this reason, it is all the more important to exercise moderation, starting with low doses and slow increments until you identify the dose that offers maximum benefit with least impact in terms of adverse effects. Clinical monitoring is also essential. It is worth repeating that the first aim is to improve quality of life and the second goal is to treat the symptoms. You should never foster any hope of curative properties among your patients; there is no clinical evidence to support such a belief.
Listed below are the chief effects of cannabinoids. Bear in mind that not all them have the same properties and actions, not all offer the effects described below and not all have the same adverse effects. Cannabinoids can be seen as real multi-purpose drugs/medicines; one composite can have several indications and uses for the same patient.
These effects are: anti-inflammatory, analgesic, neuroprotective, anticonvulsant, muscular relaxant, stimulant of bone formation and growth, anti-tumoural, antiemetic, anti-nausea, intestinal antispasmodic, appetite stimulant or suppressant, anxiolytic, antipsychotic, sleep facilitator, immunomodulator, antioxidant and as a preventer of relapse and withdrawal symptoms in chemical dependencies.
Based on these effects, potential uses are for:
- Neurological diseases:
- Epilepsy
- Neurodegenerative diseases: Alzheimer's disease, Parkinson's Disease, Multiple Sclerosis, Huntington's Chorea, Amyotrophic lateral sclerosis (Motor Neuron Disease)
- Tourette's Syndrome
- Autism
- Digestive Diseases and Diseases of Nutritional Status
- Crohn's Disease and other inflammatory conditions of the intestine
- Nausea and vomiting (associated with different clinical conditions)
- Anorexia – Cachexia
- Skin diseases
- Dermatitis
- Itching
- Acne vulgaris
- Mental Health and Addiction Disorders
- Post-Traumatic Stress Disorder
- Anxiety
- Insomnia
- Chemical addictions
- Pain:
- Chronic
- Neuropathic
- Metastatic
- Migraine
- Fibromyalgia
- Autoimmune Diseases:
- Psoriasis
- Systemic lupus erythematosus
- Scleroderma
- Rheumatoid arthritis
- Type I Diabetes
- Open angle glaucoma
- Bone Diseases:
- Osteoporosis
- Cancer and Palliative Care:
- Side effects of chemotherapy, especially nausea, vomiting, general malaise and pains
- Coadjuvant of chemotherapy
- HIV/AIDS
- Hepatitis C
- Accompaniment in terminal stages due to multiple causes
TABLE 1 - ADVERSE EFFECTS
- Generally slight to moderate in importance and will diminish without any specific treatment
- No lethal cases have been reported with cannabis (the same is not true of synthetic cannabinoids sold on the clandestine market)
- When adverse effects do occur, they may be easily reversed by reducing the dose of cannabinoids or the associated medication depending on the case
- The possibility of bimodal effect should be taken into account: i.e. at certain doses they may have one effect and at others the opposite (dose-response curve)
The adverse effects are:
- Tiredness
- Sleepiness
- Dizziness
- Nausea
- Tachycardia, hypertension or hypotension (care should be taken in patients with cardiovascular antecedents)
- Orthostatic hypotension
- Dry mouth and reduced lacrimation
- Muscle relaxation (may be a desired therapeutic effect in cases of spasticity)
- Motor-coordination disorders
- Memory and concentration disorders
- Increased appetite (may be a desired effect in some clinical cases such as in anorexia of different causes)
- Hypoglycemia
Recommended scientific reading
- Grotenhermen F, Russo E (Eds). Cannabis and Cannabinoids: Pharmacology, Toxicology, and Therapeutic Potential. New York, New York: Routledge Publishing (Imprint of Taylor & Francis Group), 2002.
- Mechoulam R (Ed). Cannabinoids as Therapeutics. Basel, Switzerland: Birkhäuser Publishers (Imprint of Springer Science+Business Media), 2005.
- Onaivi ES, Sugiura T, Di Marzo V (Eds). Endocannabinoids: The Brain and Body's Marijuana and Beyond. Boca Raton, Florida: CRC Press (Imprint of Taylor & Francis Group, Publishers), 2006.
- The Handbook of Cannabis Therapeutics: From Bench to Bedside (Haworth Series in Integrative Healing). E. Russo and F. Grotenhermen Eds. Julio, 2006.
- El Sohly MA (Ed). Marijuana and the Cannabinoids. Totowa, New Jersey: Humana Press, 2007.
- Integrative Oncology - Donald I. Abrams and Andrew T. Weil, Eds. - Oxford University Press, March, 2009
- The Medicalization of Cannabis. The transcript of a Witness Seminar held by the Wellcome Trust Centre for the History of Medicine at UCL, Crowther S M, Reynolds L A, Tansey E M. London, 2010
- Di Marzo V. Cannabinoids. Hoboken, New Jersey: Wiley-Blackwell, 2014.
- Handbook of Cannabis, Ed. Roger Pertwee, Ed. - Oxford University Press, October, 2014
- Di Marzo V, Wang J (Eds). The Endocannabinoidome: The World of Endocannabinoids and Related Mediators. Cambridge, Massachusetts: Academic Press (Imprint of Elsevier), 2014.
- Fattore L (Ed). Cannabinoids in Neurologic and Mental Disease. Cambridge, Massachusetts: Academic Press (Imprint of Elsevier), 2015.