By Ester Aso

PhD in Biology from the Universitat Pompeu Fabra, currently performing the tasks of Associate Professor of Pharmacology at the University of Barcelona. Her research work has focused over the last 15 years on the study of the role of the endocannabinoid system in mental illness and, especially, on the therapeutic potential of cannabinoids against neurodegenerative diseases such as Alzheimer's. As a result of this research, she has published 20 scientific articles related to cannabinoids and has participated in numerous research projects financed by public and private funds. Member of the Spanish Society of Research on Cannabinoids since 2004, she was a member of the Board of Directors from 2011 to 2 105.
Over the past 15 years, scientific evidence has been accumulating, most of it obtained from experimental models, which support the hypothesis that certain cannabinoids may be beneficial for the treatment of Alzheimer's disease. This paper summarises this evidence and sets out the challenges ahead and future prospects in this promising field of research.
Alzheimer's disease
Alzheimer's disease is the most common form of dementia in old age. It is estimated that it currently affects some 50 million people around the world and that this figure could double every 20 years, mainly due to the continued growth of life expectancy in our society [1]. It is a highly incapacitating disease characterized by a progressive deterioration of cognitive and mental abilities. Initially it causes problems remembering words, conversations or recent events and may be combined with apathy and depression. As the disease progresses, the patient suffers problems communicating, widespread confusion, spatial and temporal disorientation and behavioural changes that may include aggressiveness. Approximately 10 years after the onset of these symptoms, physical deterioration is usually very advanced, requiring continued attention for all daily activities, and inevitably leads to the death of the patient. The long process of the disease involves an enormous emotional cost to the patient and his or her relatives and an enormous economic cost to the health and social care systems.
Despite the numerous efforts made in the field of pharmacological research against Alzheimer's disease in the past 30 years, today the only treatments available may produce discrete improvements at the cognitive and functional level but in no way halt or reverse the neurodegenerative process associated with Alzheimer's disease [2]. Due to the limitations of these drugs, there is an alarming need for more effective therapeutic options to address the growing population affected by this dementia.
In this sense, the scientific community is working hard to find new therapies that can reduce the impact of this disease. There are currently up to 400 active clinical trials to evaluate different experimental treatments, oriented in general to alleviate some of the molecular alterations that have been described in the course of Alzheimer's disease. Among the therapeutic strategies evaluated are those designed to reduce the toxicity of the beta-amyloid peptide (Aβ) and the hyperphosphorylation of the tau protein, the two most characteristic pathological events of the disease, which have been related to neuronal death and the consequent progressive deterioration of mental functions [3]. In addition, other experimental therapies are trying to assess if the reduction of the inflammatory process and oxidative stress that accompanies the accumulation of Aβ in the form of extracellular plaques and the formation of neurofibrillary tangles of hyperphosphorylated tau in the patient's brain, might prevent the progress of the disease. However, to date, none of these experimental approaches have been completely satisfactory and the approval of new drugs for the treatment of Alzheimer's is not anticipated in the short term.
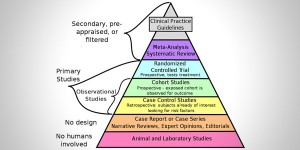
The failure of these therapeutic strategies may be due to the fact that in many cases they have been tested in patients at moderate or advanced stages of the disease, when the possibilities for reversal of the neurodegenerative process are more limited. Therefore, the search for markers of early detection of the disease has become another fundamental pillar of the research into Alzheimer's disease, as it should facilitate intervention at the early stages of the neurodegenerative process and thus increase the chances of success. But in addition, it is likely that the fact that most of these experimental therapies tested in patients to date have been designed to act specifically only on a single pathological event of the many that occur sequentially or in parallel during the onset of Alzheimer's disease has also contributed to this failure, so the complexity of pathology as a whole has not been addressed.
For this reason, a new scientific trend advocates the search for new multiple target therapies against Alzheimer, which are capable of simultaneously modulating the main pathological events that determine the progressive functional deterioration of patients. In this context, the therapeutic potential of cannabinoids against this disease has been gaining increasing interest, supported by increasing evidence demonstrating an improvement in Alzheimer-type symptomatology in various models of the disease after exposure to these compounds. This improvement would be associated with cannabinoid-induced modulation of both processes associated with Aβ and tau hyperphosphorylation and inflammation and oxidative stress, among others, as described in the following paragraphs and in some scientific reviews on the subject [4, 5].
The endocannabinoid system in Alzheimer's disease
Early evidence that cannabinoid compounds might be useful against Alzheimer's was obtained from the study of the composition of the endocannabinoid system (consisting of receptors on which cannabinoids, endogenous ligands and enzymes responsible for the synthesis and degradation of these ligands act), in post-mortem samples of brains of patients suffering from the disease. Thus, the research groups of Dr. Julián Romero and Dr. María de Ceballos, both located in Madrid, pioneered the description of the increase in the expression of the cannabinoid receptor CB2 in the microglia cells (charged with modulating inflammatory processes in the brain, among other defensive functions) that are activated around the amyloid plates characteristic of Alzheimer's. These observations were subsequently corroborated by other researchers and animal models of the disease. Similarly, it is widely demonstrated and accepted that in focal points of inflammation associated with Aβ plates there is an increase in the fatty acid expression of amide hydrolase (FAAH), the enzyme responsible for the degradation of endogenous cannabinoid ligand anandamide [6]. These findings support the hypothesis that the CB2 receptor and FAAH may be interesting pharmacological targets in the fight against Alzheimer's [6, 7].
There is, on the other hand, some controversy over the affect in Alzheimer's of the levels of the cannabinoid receptor CB1, abundantly expressed in the brain and with important functions in the homeostatic control of neuronal activity under physiological conditions. Some studies have shown an increase in the activity of this receptor at early stages of the disease, followed by a marked reduction in its levels at advanced stages [8]. However, other studies have not been able to find significant differences in CB1 levels between the brains of people with Alzheimer's disease and those of healthy people [9]. However, this controversy does not reduce the interest in modulating CB1 receptor activity in Alzheimer cases, given its neuroprotective character and its involvement in numerous processes that are affected during the course of the disease. In fact, a recent study carried out by our research group showed that this receptor plays a fundamental role in the progression of Alzheimer's as its elimination, through genetic manipulation techniques, leads to an acceleration of the degenerative process and leads to premature death in an animal model of the disease [10].
Clinical and preclinical evidence of the usefulness of cannabinoids against Alzheimer's
Most of the existing evidence on the therapeutic potential of cannabinoids has been obtained by the use of animal and cellular models that replicate some of the alterations that occur in a brain affected by Alzheimer's. However, it is worth noting that the limited clinical data obtained to date also supports the usefulness of these compounds to mitigate some of the behavioural alterations associated with Alzheimer's. Thus, the four clinical trials conducted with a small group of patients in advanced stages of the disease treated for several weeks with a Delta-9-tetrahydrocannabinol analogue (THC) resulted in a reduction in agitation and aggressiveness and an increase in body weight in patients who previously rejected food. Equally important, the adverse effects associated to treatment with cannabinoids described in these early clinical trials were limited to euphoria, drowsiness, and fatigue, without requiring the interruption of treatment in any of the patients, which indicates that the analogues of the THC may have an acceptable safety profile for use in patients of advanced age (reviewed in [11]).
As mentioned above, it has been the results obtained in experimental models of the disease that have contributed the most evidence on the potential usefulness of cannabinoids in Alzheimer's. Thus, numerous in vitro and in vivo studies have shown that the stimulation of CB1 and CB2 receptors, either by endogenous ligands, synthetic or natural cannabinoids (THC and cannabidiol or CBD), reduces the neural toxicity of peptide Aβ, increasing the viability of neurons in culture and protecting from cognitive impairment induced by this peptide in animals inoculated with it or genetically manipulated to express it abundantly. It is important to note that in all cases the doses of cannabinoids that have been tested in experimental models have been much lower than those that produce the characteristic psychoactive effects of cannabis use. This neuronal protection against the peptide Aβ could be associated on the one hand with the ability of cannabinoids with activity at the CB2 receptor to promote the elimination of this peptide and to reduce the signalling pathways activated by Aβ that lead to cell death, and on the other to the stimulation of neurogenesis (formation of new neurons) and the maintenance of synaptic boutons, which are crucial for correct communication between the neurons [4, 5].
In addition, the neuroprotective effect of cannabinoids against Aβ would also be associated with their ability to mitigate other harmful effects induced by this peptide beyond the directly toxic effect on neurons. Thus, the inflammatory response triggered by the presence of the peptide Aβ, which when it becomes chronic is harmful to the brain tissue, is reduced after administration of cannabinoids that stimulate the CB2 and also the CB1 receptor, such as THC, endocannabinoids, or some synthetic agonists. Likewise, CBD, whose mechanism of action is not completely elucidated, has anti-inflammatory properties in models of Alzheimer's disease. Similarly, some evidence points to a reduction in oxidative stress induced by peptide Aβ following the administration of CBD, THC and synthetic agonists of the CB2 receptor, so that they would contribute to the protection of the cellular structures most vulnerable to oxidative damage and thus preserve their functionality [4, 5].
Other additional benefits that would result from the use of cannabinoids in Alzheimer's disease would be, according to preclinical studies, an improvement in vascular dysfunction characteristic of this dementia and the ability to absorb glucose, favouring the supply of oxygen and nutrients needed for normal brain functioning. In addition, certain cannabinoids with CB1 receptor activity may regulate neurotransmission, either by modulating the same therapeutic targets as the drugs currently approved for the treatment of Alzheimer's disease, or by modulating the balance between excitatory and neuronal inhibitory activity, which is compromised during the neurodegenerative process associated with Alzheimer's disease. Finally, it should be noted that there is evidence that certain natural or synthetic agonists of the CB1 receptor and CBD are capable of reducing tau hyperphosphorylation in both cultured and animal cells [4, 5].
All these effects together would contribute to the cognitive improvement observed following administration of natural cannabinoids, including THC and CBD [12], or synthetics in several animal models of the disease.
Outstanding challenges and future prospects
Considering all the scientific evidence mentioned above and the complexity of Alzheimer's disease, it seems clear that the ability of cannabinoids to modulate in parallel many of the alterations that occur during the course of this disease potentially gives them a therapeutic advantage over current treatments and other experimental drugs aimed at modifying a single pathological event. Based on current knowledge, the optimal approach would be the use of combinations of cannabinoids that had activity on CB1 and CB2 receptors, such as THC, and also incorporated other compounds with complementary activity, such as CBD. However, despite the promising preclinical results achieved to date, there are still a number of outstanding challenges that require intensive research in the future to bring this therapeutic alternative closer to the patient with guarantees. First, it will be essential to know in more detail the mechanisms of action of these cannabinoid compounds in animal models of Alzheimer's to try to optimize future therapies. Secondly, progress needs to be made in clinical research with patients, which will undoubtedly be the greatest challenge. This will require the design of controlled clinical trials assessing the efficacy but also the safety of cannabinoids in a sufficient number of patients to allow statistically significant conclusions to be drawn. It would be desirable to consider first of all patients in the early stages of this disease in order to increase the chances of success. All of this requires the commitment, effort and coordination of all the actors involved: researchers, health personnel, patients, cannabinoid producers and funding agencies. The task is arduous, but highly motivating.
References
[1] Alzheimer's Association. 2017 Alzheimer's Disease. Facts and Figures. Alzheimer's & Dementia, 2017 13:325-73.
[2] Howard R, McShane R, Lindesay J, et al. Donepezil and memantine for moderate-to-severe Alzheimer's disease. N Engl J Med. 2012 366:893-903.
[3] Bloom GS. Amyloid-β and tau: the trigger and bullet in Alzheimer disease pathogenesis. JAMA Neurol. 2014 71:505-8
[4] Aso E, Ferrer I. Cannabinoids for treatment of Alzheimer's disease: moving toward the clinic. Front Pharmacol. 2014 5:37
[5] Aymerich MS, Aso E, Abellanas MA, Tolon RM, Ramos JA, Ferrer I, Romero J, Fernández-Ruiz J. Cannabinoid pharmacology/therapeutics in chronic degenerative disorders affecting the central nervous system. Biochem Pharmacol. 2018 157:67-84.
[6] Benito C, Núñez E, Tolón RM, Carrier EJ, Rábano A, Hillard CJ, Romero J. Cannabinoid CB2 receptors and fatty acid amide hydrolase are selectively overexpressed in neuritic plaque-associated glia in Alzheimer's disease brains. J Neurosci. 2003 23:11136-41.
[7] Aso E, Ferrer I. CB2 Cannabinoid receptor as potential target against Alzheimer's disease. Front Neurosci. 2016 10:243.
[8] Manuel I, González de San Román E, Giralt MT, Ferrer I, Rodríguez-Puertas R. Type-1 cannabinoid receptor activity during Alzheimer's disease progression. J Alzheimers Dis. 2014 42:761-6.
[9] Mulder J, Zilberter M, Pasquaré SJ, Alpár A, Schulte G, Ferreira SG, Köfalvi A, Martín-Moreno AM, Keimpema E, Tanila H, Watanabe M, Mackie K, Hortobágyi T, de Ceballos ML, Harkany T. Molecular reorganization of endocannabinoid signalling in Alzheimer's disease. Brain. 2011 134:1041-60.
[10] Aso E, Andrés-Benito P, Ferrer I. Genetic deletion of CB(1) cannabinoid receptors exacerbates the Alzheimer-like symptoms in a transgenic animal model. Biochem Pharmacol. 2018 157:210-216.
[11] Krishnan S, Cairns R, Howard R. Cannabinoids for the treatment of dementia. Cochrane Database Syst Rev. 2009 2:CD007204.
[12] Aso E, Sánchez-Pla A, Vegas-Lozano E, Maldonado R, Ferrer I. Cannabis-based medicine reduces multiple pathological processes in AβPP/PS1 mice. J Alzheimers Dis. 2015 43:977-91.