By Manuel Guzmán
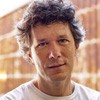
Manuel Guzmán is Professor of Biochemistry and Molecular Biology at Complutense University of Madrid, member of the Spanish Royal Academy of Pharmacy, and member of the Board of Directors of the International Association for Cannabinoid Medicines. His research focuses on the study of the mechanism of action and therapeutic properties of cannabinoids, especially in the nervous system. This work has given rise to more than one hundred publications in specialized international journals, as well as to several international patents on the possible therapeutic applications of cannabinoids as anticancer and neuroprotective drugs. He routinely collaborates with scientific reviewing and funding agencies.
For several decades now, many research groups around the world, including some Spaniards, have been forging a very high-level medical chemistry around the endocannabinoid system, which has provided numerous synthetic cannabinoids (sometimes referred to as "sintocannabinoides" in Spanish) that today constitute day very useful pharmacological tools for preclinical studies that we usually perform in our laboratories with cells and experimental animals. However, these enormous efforts have so far failed to bring effective and safe medications to clinical practice for the benefit of patients. Below are some of the most salient examples of this.
1. Direct activators of cannabinoid receptors
In recent years, several compounds (called "agonists" in pharmacology) have been designed to bind with the CB1 cannabinoid receptor and strongly activate it. The most representative case is nabilone (Cesamet®), marketed by Valeant Pharmaceuticals and approved in the mid-1980s by the US Food and Drug Administration for the treatment of nausea and vomiting associated with cancer chemotherapies and the syndrome of attrition (cachexia) associated with AIDS. However, the clinical use of this substance and the studies carried out with other similar compounds have shown very limited therapeutic windows due to notorious psychoactive effects, which is why they are not usually well tolerated by patients at therapeutically effective doses.
Selective activators of the CB2 cannabinoid receptor, such as those originally designed by Prof. Raphael Mechoulam at the Hebrew University of Jerusalem (in collaboration with the Pharmos company - nowadays Yissum-) are compounds with adequate tolerability as they are free of the unwanted psychoactive effects that the CB1 receptor mediates in our brain. However, until now they have failed, because of their reduced efficacy, to find their pharmacological route beyond small phase II studies, for example in the field of pain treatment.
2. Direct blockers of cannabinoid receptors
The opposite pharmacological strategy has also been pursued, that is the use of substances (called "antagonists" in pharmacology) that bind to the cannabinoid CB1 or CB2 receptor and block their activity. The most extensive clinical studies conducted with selective CB1 receptor antagonists have been especially aimed at preventing the activation of ingestion and anabolism (for example, synthesis and storage of lipids) that the endocannabinoid system mediates through said receptor in order to fight obesity. However, the resounding failure of rimonabant (Acomplia®, from the company Sanofi-Aventis, which was approved by the European Medicines Agency, but not by the US Food and Drug Administration) and the result of its serious adverse effects on the mental health of some patients, scuttled the CB1 receptor blocker development programs that many pharmaceutical companies had underway. No one has tried, for the moment, to bring selective CB2 receptor antagonists into the clinic.
3. Indirect activators of cannabinoid receptors
Endocannabinoids are actively synthesized by neurons and other cells in our body and, when they have exerted their biological action, they are degraded and deactivated by specific enzymes. Therefore, blocking these enzymes increases the levels of endocannabinoids (and, therefore, the activity of cannabinoid receptors) in specific locations in our body. This pharmacological strategy has already been applied to other chemical mediators of our brain, for example in the treatment of psychiatric disorders by mediating selective inhibitors of monoamine deactivation. In recent years, the action of various enzyme inhibitors that degrade endocannabinoids has been studied clinically. However, a few years ago the fatal outcome (one dead and five seriously ill) of a clinical trial conducted with the compound BIA 10-2474, a drug synthesized by the company Bial-Portela that inactivates the enzyme that degrades the endocannabinoid anandamide (the so-called "fatty acid amide hydrolase", generally abbreviated as FAAH - from the English fatty acid amide hydrolase) was announced in France. Although the lethal effect of the compound was probably not caused by the elevation of anandamide levels but by its collateral action on other as yet unidentified molecular targets, the "BIA case 10-2474" may make it very difficult for FAAH inhibitors developed by other companies to prosper, at least in the near future.
In the midst of this bleak clinical scenario of sintocannabinoids, patients must use well-purified plant cannabinoids such as THC or CBD (sometimes called "phytocannabinoids"), or, most commonly, raw cannabis preparations. Hopefully in the future we will have a more complete arsenal of molecules that act pharmacologically on the endocannabinoid system to increase the therapeutic benefit for patients. However, the ubiquity of the endocannabinoid system, the lipid nature of its ligands (the endocannabinoids) and the biological complexity of its actions are some of the factors that make this a titanic objective, especially as any potential cannabinoid drug synthesis must be "competitive" in terms of efficacy, safety and economic cost compared to Cannabinoids extracted from Cannabis sativa. The recent elucidation of the precise three-dimensional structure of the CB1 receptor, both in its active form (that is, linked to a receptor agonist) and in its inactive form (that is, linked to a receptor antagonist), opens a door to rationally designed sintocannabinoids with more polished therapeutic properties than those achieved so far.


